Out-of-Network Behavioral Health Claims Process
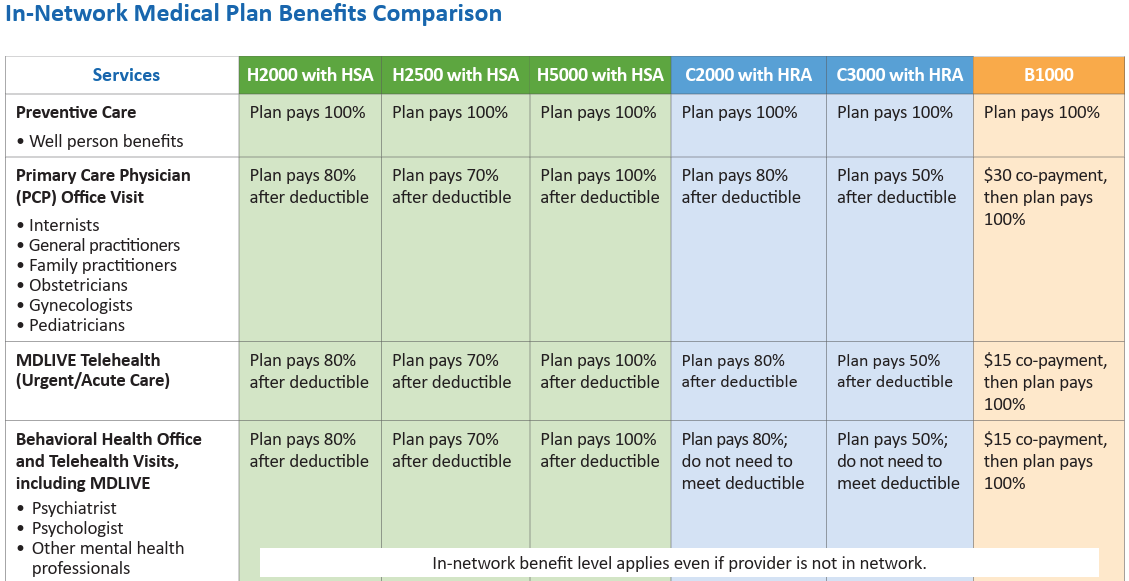
HealthFlex covers out-of-network mental health counseling at the same benefit level as in-network whether your provider is in-network or not. As discussed on the HealthFlex Behavioral Health Webinar (slides pdf), if your provider is out-of-network, you may not be able to take advantage of the BCBS network discount and you may have to pay upfront, submit a claim and wait for reimbursement, but your actual benefit level will be the same. See the current HealthFlex Plan Comparison to find the in-network behavioral health visit co-insurance amount for your current health plan that will be applied to your out-of-network services.
If you are seeing an out-of-network provider, please read and complete this claim form for submitting your claims for reimbursement. TIP: in Part 3 of the form enter the service date and “ongoing mental health treatment” as the type of treatment received. Please make sure that your receipt includes all of the necessary information before emailing to ADMMemberSubmittedClaims@bcbsil.com. Contact your Care Coordinator at (833) 762-0876 with questions.
HealthFlex 2025
HealthFlex Plan Comparisons 2025 (Korean | Spanish)
How Do I Choose My HealthFlex Plans 2025 (Korean | Spanish)
Have You Called Your Care Coordinator?
Wespath Care Coordinators are ready and waiting to help HealthFlex participants navigate their health care journey for 2024. Care Coordinators are available at (833) 762-0876, Monday-Friday, 8:30 a.m.- 10:00 p.m., Eastern. Primary participants and adult dependents can access their Care Coordination account now at mywespathhealth.com and message or chat with a Care Coordinator. Participants will also be able to access their account via Benefits Access soon.
Care Coordinators are your personal team of nurses and benefits experts working with you and your providers to make your care simpler and more affordable. Care Coordinators can help you with anything related to your health care and benefits—especially items related to your medical, pharmacy, and behavioral health benefits. Whether you have a question about your claims or bills, need help knowing what’s covered under your health plan, can’t remember how to submit a manual claim, want to prepare for an upcoming doctor’s visit, or just need a new ID card, Care Coordinators are here for you.
No request is too big or too small for your Care Coordinators. They will do whatever it takes to help you understand and use your health benefits.
Watch this short video and read these FAQs to learn more about how Care Coordination can help you.
Golden Cross and One Who Is Loved Benevolent Grants Available
The Golden Cross Benevolent Fund supports the laity of any age in our Annual Conference who are experiencing financial
difficulty due to excessive medical expenses such as hospital/physician services, dental, pharmacy, mental health, vision
needs, home health services, and medical travel expenses.
A special grant called “One Who Is Loved” makes possible love gifts to benefit children under the age of 18 who have special needs. Examples of special needs include specialized medical equipment or supplies/medicine, transportation to hospitals or treatment, or other special needs.
Pastors of the NC Conference are encouraged to recommend adults who are members of, or children (18 years old or younger) who are members of, or children who have at least one parent who is a member of, a local United Methodist Church in the NC Conference. Golden Cross grants are available for up to $2,500 per year. One Who Is Loved grants are available for up to $1,000 per year per child. Complete the application here. Applications are open year-round and subject to the availability of funds.
Donations are encouraged to enable this special grant fund to serve the needs of many children and should be directed to the United Methodist Foundation.
Post-Retirement Insurance Policies History
See the Insurance Plan History document for an historical account of the policies affecting post-retirement insurance benefits.
Blueprint For Wellness
We are excited to announce the Blueprint For Wellness (BFW) screening is returning to Annual Conference in 2025! This health screening includes a blood draw and a few measurements, such as blood pressure and waist circumference. This screening is open to enrollees (participants and spouses) on the conference’s active health insurance plans.
Attendees will receive:
- $100 in Pulse Cash in their Personify Health well-being program. This incentive reward is redeemable as a transfer to your checking account or can be redeemed for gift cards, merchandise, or a charitable donation.
- Up to 140 Wellness Credits for achieving healthy results. Earn a total of 150 Wellness Credits before the end of the year and receive an additional $150 in Pulse Cash.
- Free, personalized, confidential data on 30 health factors that can be shared by the participant with their primary care provider. Healthcare providers have indicated that this valuable information supports them in creating an overall plan for the health of their patients.
Schedule Your Blueprint for Wellness Health Screening
- Log in to your Personify Health account and find Quest Blueprint for Wellness Screening under the “Benefits” tab or through Benefits Access (for participants) under the “Well-Being” tab.
- Call Quest Diagnostics at 1-855-623-9355. Employer group = HealthFlex or United Methodist Church
Health Check
This year’s results can be entered in the Personify Health Check. When participants and their covered spouses take the Health Check they avoid a higher deductible in 2026.
To take the Health Check, log into your Personify Health account through the website or app, select the “Health” tab, and then choose “HealthCheck.”
The deadline for completing both the BFW and the Personify Health Check is August 31.
